Explore Psoriasis and what your DNA can tell you
What is psoriasis?
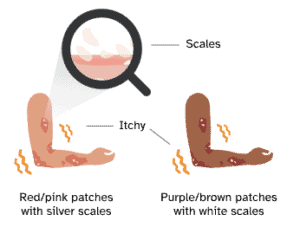
Psoriasis is a chronic autoimmune condition most commonly characterized by itchy, discolored patches covered in silvery white flakes, called “scales,” that form on the skin. Psoriasis symptoms may come and go throughout life, and certain triggers can cause them to flare up. Psoriasis is not an infection and is not contagious.
Psoriasis is a noncontagious condition that causes new skin cells to grow faster than usual. In the most common type of psoriasis, skin cells build up into thick patches called “plaques,” especially on the knees, elbows, trunk, and scalp. Plaques can look red or pink on lighter skin and brownish or purple on darker skin, and they may be covered in silvery or white flakes called “scales.” Although the causes of psoriasis are not fully understood, scientists know that an overactive immune response and inflammation play a role in the increased growth of skin cells.
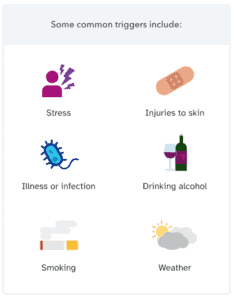
What are psoriasis triggers?
For people who have psoriasis, symptoms can come and go throughout life, but certain factors (called triggers) can increase the chances of a flare-up. Common triggers include:
- Stress. Stress can also worsen symptoms of psoriasis.
- Injuries to skin. This can include scratches, sunburns, bug bites, or needle injections.
- Illness or infection. Anything that affects the immune system can trigger flare-ups.
- Drinking alcohol. Frequent or heavy alcohol consumption can trigger flare-ups and prevent psoriasis medication from working.
- Smoking or spending time with someone who smokes.
- Weather. Most commonly, flare-ups may be triggered by cold, dry weather or intense sun exposure.
Triggers can vary from person to person. To help identify personal factors and become aware of any patterns, experts recommend tracking psoriasis triggers and symptoms. Additionally, talking to a healthcare professional like a dermatologist may help in identifying and managing triggers.
How can psoriasis impact your health?
Although scientists don’t fully understand why, psoriasis is associated with an increased risk for other health conditions. Around 40% of people with psoriasis experience psoriatic arthritis, which is pain, swelling, and stiffness in the joints that can result in permanent damage. In addition, people with psoriasis have a higher chance of developing high blood pressure, diabetes, heart disease, and other autoimmune conditions. Although there is no cure for psoriasis, there are many promising treatment options for managing symptoms and reducing the risk of developing other health conditions. If you have concerns about psoriasis or would like to seek treatment, talk to a healthcare professional.
Because psoriasis can be visible and cause chronic discomfort, it can also impact mental health. Individuals with psoriasis may experience feelings of low self-esteem, depression, or anxiety. Counseling and/or support groups can be an important part of some psoriasis management plans.

Is psoriasis genetic?
Genetics do play a role in psoriasis. This means some people may be more likely to develop psoriasis than others, depending on their genetics. A person has an increased chance of developing psoriasis if one parent has it, and an even higher chance if both parents have psoriasis. In most cases, it is a combination of many different genetic variants that impact a person’s chances of developing psoriasis. Individually, each of these variants only has a small impact on a person’s genetic likelihood, but that impact can grow when many variants are considered together. 23andMe takes into account more than 7,500 genetic markers to estimate the likelihood of developing psoriasis, but keep in mind that other factors besides genetics can also influence a person’s overall likelihood of developing psoriasis.
Other factors that may cause an increased likelihood of psoriasis
It is estimated that about 7.5 million Americans have psoriasis. Besides genetics, some factors that can increase a person’s chances of developing psoriasis include:
- Family history
- Certain health conditions (including diabetes and high blood pressure)
- Certain medications (including beta-blockers, lithium, and antimalarial drugs; medications can also trigger psoriasis flare-ups)
Find out if your genetics might increase your likelihood of developing Psoriasis
Curious whether you have an increased likelihood of developing psoriasis based on your genetics? Find out more with the Psoriasis report (Powered by 23andMe Research), part of the 23andMe+ Premium membership. 23andMe+ Premium includes our Health + Ancestry Service plus new premium reports and features throughout the year.

23andMe+ Premium
Please note:
- This report does not diagnose psoriasis and should not be used to make medical decisions.
- The report was developed by 23andMe scientists using data and insights gathered from thousands of customers who consent to participate in our research. Reports based on 23andMe research provide an estimate of your likelihood of developing a condition based on your genetics and other factors. This report does not account for lifestyle or family history.
- The report does not account for every possible genetic variant that could affect your likelihood of developing psoriasis.
References:
Amin M et al. (2020). “Psoriasis and Co-morbidity.” Acta Derm Venereol. 100(3):adv00033.
Kamiya K et al. (2019). “Risk Factors for the Development of Psoriasis.” Int J Mol Sci. 20(18).
Mayo Clinic. “Psoriasis.” Retrieved March 1, 2022 from https://www.mayoclinic.org/diseases-conditions/psoriasis/symptoms-causes/syc-20355840.
National Psoriasis Foundation. “About Psoriasis.” Retrieved March 1, 2022 from https://www.psoriasis.org/about-psoriasis/.
National Psoriasis Foundation. “Treating Skin of Color.” Retrieved March 1, 2022 from https://www.psoriasis.org/advance/treating-skin-of-color/.
Rendon A et al. (2019). “Psoriasis Pathogenesis and Treatment.” Int J Mol Sci. 20(6).
